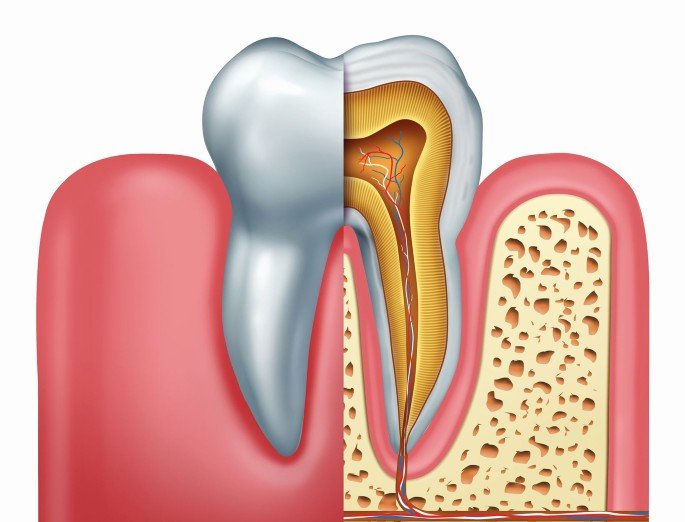
Endodontics, often referred to as “endo,” is a specialized branch of dentistry that focuses on the study and treatment of the dental pulp and the tissues surrounding the roots of teeth. The term “endodontic” is derived from the Greek words “endo,” meaning “inside,” and “odont,” meaning “tooth.”
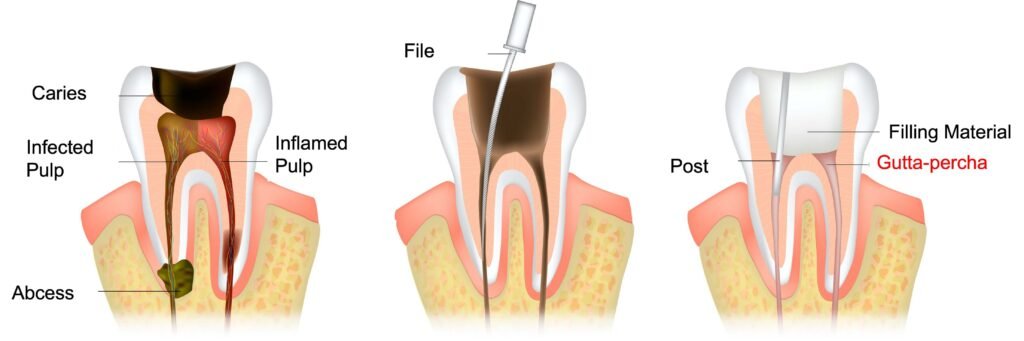
One of the most common procedures performed in endodontics is root canal treatment. This procedure involves the removal of infected or damaged dental pulp from the inside of the tooth. The dental pulp is a soft tissue that contains nerves, blood vessels, and connective tissue. When the pulp becomes infected or inflamed due to deep decay, tooth fracture, or trauma, it can cause severe pain and lead to dental abscesses if left untreated.
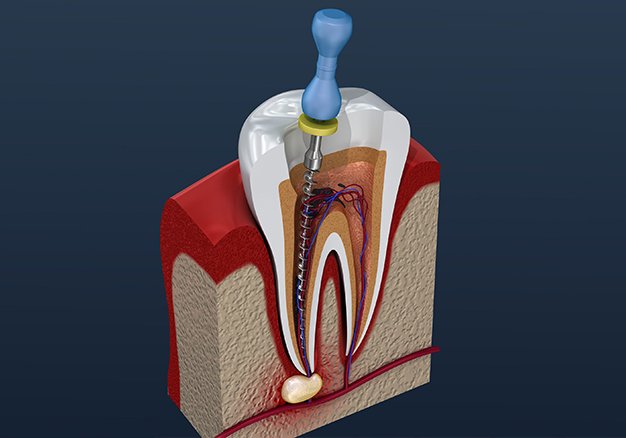
During a root canal procedure, the dentist or an endodontist carefully removes the infected pulp, cleans and disinfects the root canals, and then fills and seals them with a dental material called gutta-percha. This process helps to eliminate the infection and prevent further damage to the tooth. The procedure is typically performed under local anesthesia to ensure patient comfort.
Root canal treatment is a crucial procedure for saving teeth that would otherwise require extraction. By removing the infected pulp and sealing the root canals, the tooth can be preserved and continue to function properly. Without treatment, the infection can spread to the surrounding tissues and even affect neighboring teeth.
After a root canal treatment, a dental crown is often placed on the tooth to provide additional strength and protection. The crown helps to restore the tooth’s natural appearance and function. It also helps to prevent any further damage to the tooth, ensuring its long-term success.
In addition to root canal treatment, endodontics encompasses other procedures such as endodontic retreatment and endodontic surgery. Endodontic retreatment involves re-treating a tooth that has previously undergone root canal treatment but has developed new issues. This procedure allows the dentist or endodontist to address any persistent infection or complications.
Endodontic surgery, on the other hand, involves surgical procedures that target the root tip. This may be necessary in cases where the root canal treatment alone is not sufficient to resolve the issue. Endodontic surgery can help save a tooth by removing any infected tissue or repairing damage to the surrounding bone.
Endodontists are dentists who have undergone additional specialized training in endodontics. They are experts in performing root canal treatments and other endodontic procedures. If you require endodontic treatment, your general dentist may refer you to an endodontist for specialized care.
Overall, endodontics plays a vital role in preserving natural teeth and maintaining oral health. Root canal treatment, along with other endodontic procedures, helps to eliminate infection, alleviate pain, and save teeth from extraction. If you are experiencing dental pain or suspect an issue with your dental pulp, it is essential to seek prompt dental care to prevent further complications.
endodontics:
- Diagnosis: Endodontists use various diagnostic techniques to assess the condition of the dental pulp and identify any issues. This may include reviewing the patient’s dental history, performing a clinical examination, and using imaging techniques such as X-rays or cone beam computed tomography (CBCT) scans to visualize the internal structures of the tooth.
- Causes of Pulp Damage: Dental pulp can become damaged or infected due to several reasons, including deep tooth decay, repeated dental procedures on the same tooth, cracks or fractures in the tooth, trauma to the tooth, or gum disease that has spread to the root canals.
- Symptoms: Common symptoms that may indicate the need for endodontic treatment include persistent toothache, sensitivity to hot or cold temperatures, swelling or tenderness around the tooth, pain while chewing, or a darkening of the tooth.
- Root Canal Procedure: A typical root canal treatment involves several steps. After numbing the area with local anesthesia, the dentist or endodontist creates an access opening in the tooth to reach the pulp chamber and root canals. The infected or damaged pulp is then carefully removed using specialized instruments, and the canals are cleaned and shaped. They are then filled with a biocompatible material called gutta-percha and sealed to prevent reinfection. A temporary filling may be placed initially, and a dental crown is often recommended to restore the tooth’s strength and protect it from future damage.
- Success Rate: Root canal treatments have a high success rate and are generally effective in saving the natural tooth. With proper care, such as good oral hygiene practices and regular dental check-ups, a treated tooth can last a lifetime.
- Advancements in Endodontics: Endodontics has seen advancements in techniques and technologies in recent years. These include the use of digital imaging for more accurate diagnoses, the introduction of rotary instruments for more efficient cleaning and shaping of the root canals, and the use of operating microscopes for enhanced visualization during procedures.
Endodontics plays a crucial role in preserving natural teeth and relieving dental pain caused by pulp infections or damage. If you suspect that you may require endodontic treatment, it is recommended to consult with a dentist or endodontist who can evaluate your condition and provide appropriate care.

While root canal treatments are generally safe and successful, there are some potential complications and risks associated with the procedure. It’s important to note that these complications are relatively rare, and most patients experience a smooth and problem-free recovery. However, here are a few potential complications:
- Infection: In some cases, the treated tooth may not heal properly, leading to persistent or recurrent infection. This can occur if the root canals are not thoroughly cleaned, if there are additional undetected canals, or if bacteria re-enter the tooth after the procedure. In such cases, a retreatment or additional endodontic intervention may be necessary.
- Instrument Fracture: During the root canal procedure, endodontic instruments are used to clean and shape the canals. In rare instances, these instruments may fracture or break within the tooth, making their retrieval challenging. If the fractured instrument cannot be removed, it may be left in place as long as it does not compromise the success of the treatment.
- Perforation: While accessing and cleaning the root canals, there is a small risk of inadvertently creating a perforation or a tiny hole in the root or the surrounding structures. If a perforation occurs, it may require repair through a surgical procedure or other specialized techniques.
- Tooth Discoloration: In some cases, a treated tooth may change color and appear darker compared to the surrounding teeth. This can happen due to the breakdown of blood products or the presence of certain medications used during the procedure. Tooth discoloration can often be addressed through various cosmetic dental treatments.
- Cracked Tooth: Root canal-treated teeth can become more fragile over time. In rare instances, a tooth may develop a crack or fracture, especially if it was already weakened before the procedure. A cracked tooth may require additional dental treatments, such as a crown or a dental extraction.
It’s important to discuss any concerns or potential risks with your dentist or endodontist before undergoing a root canal treatment. They can provide you with personalized information based on your specific dental situation and address any questions or uncertainties you may have.
Endodontic gutta-percha is a material commonly used in root canal treatments. It is a rubbery, thermoplastic material that is biocompatible and inert, meaning it does not cause adverse reactions within the body.
After the infected or damaged dental pulp is removed during a root canal procedure, the root canals need to be filled to prevent reinfection. Gutta-percha is the primary material used for this purpose. It is placed inside the cleaned and shaped root canals to seal them off and create a barrier against bacteria.
Here are some key features and benefits of endodontic gutta-percha:
- Biocompatibility: Gutta-percha is well-tolerated by the body and does not cause significant immune responses or irritation. It is considered safe for use in dental procedures.
- Thermal Plasticity: Gutta-percha can be softened by heating, making it malleable and allowing it to conform closely to the shape of the root canals. Dentists use heat sources, such as warmers or handheld heat carriers, to soften the gutta-percha before placement.
- Sealing Ability: The thermoplastic nature of gutta-percha, combined with its ability to flow when heated, enables it to effectively seal the root canals. This sealing action helps to prevent bacteria from re-entering the tooth and causing reinfection.
- Radiopacity: Gutta-percha is radiopaque, which means it can be easily seen on dental X-rays. This property allows dentists to confirm the proper placement and filling of the root canals during and after the procedure.
- Longevity: Gutta-percha is a durable material that provides long-term stability and sealing within the root canals. When combined with an appropriate dental sealer, it helps to maintain the integrity of the treated tooth.
It’s worth noting that gutta-percha is typically used in conjunction with root canal sealers, which are cement-like materials that enhance the sealing properties and fill any remaining gaps within the root canal system.
Overall, gutta-percha is a crucial component of endodontic treatment and plays a significant role in the success and longevity of root canal procedures. Its biocompatibility, thermal plasticity, sealing ability, and radiopacity make it an ideal choice for filling and sealing the root canals, thereby preserving the treated tooth.

Several root canal sealers are commonly used in conjunction with gutta-percha during endodontic procedures. These sealers help to enhance the sealing properties of gutta-percha and ensure the complete filling of the root canal system. Here are some common types of root canal sealers:
- Zinc Oxide-Eugenol (ZOE) Sealers: ZOE sealers have been used for many years and are known for their antimicrobial properties. They contain a mixture of zinc oxide and eugenol, which provides sedative and antibacterial effects. ZOE sealers have a relatively long setting time and may require a longer waiting period before the final restoration is placed.
- Calcium Hydroxide Sealers: Calcium hydroxide-based sealers contain calcium hydroxide mixed with a resin component. These sealers have antimicrobial properties and promote the formation of hard tissue (dentin bridge) in cases of periapical inflammation. They have a long setting time and may require multiple appointments for complete root canal filling.
- Epoxy Resin Sealers: Epoxy resin-based sealers consist of epoxy resin and a hardening agent. They are known for their excellent sealing ability and dimensional stability. Epoxy resin sealers have a relatively short setting time and provide a strong bond to dentin. They are widely used in modern endodontics.
- Bioceramic Sealers: Bioceramic sealers are newer additions to the field of endodontics. They are composed of calcium silicates, calcium phosphates, and other bioactive components. Bioceramic sealers have excellent sealing ability, biocompatibility, and antimicrobial properties. They also have the ability to form a hydroxyapatite-like material, which can aid in the healing of periapical tissues.
It’s important to note that the choice of sealer depends on various factors, including the specific clinical situation, properties of the sealer, and the preferences and experience of the treating dentist or endodontist. Each sealer has its own advantages and considerations, and the selection is typically based on the specific needs of the patient and the desired treatment outcome.

Furthermore, it’s worth mentioning that advancements and research in endodontics continue to introduce new sealers and materials with improved properties and performance. Dentists and endodontists stay updated with the latest developments in the field to provide the most effective and appropriate treatment options for their patients.
